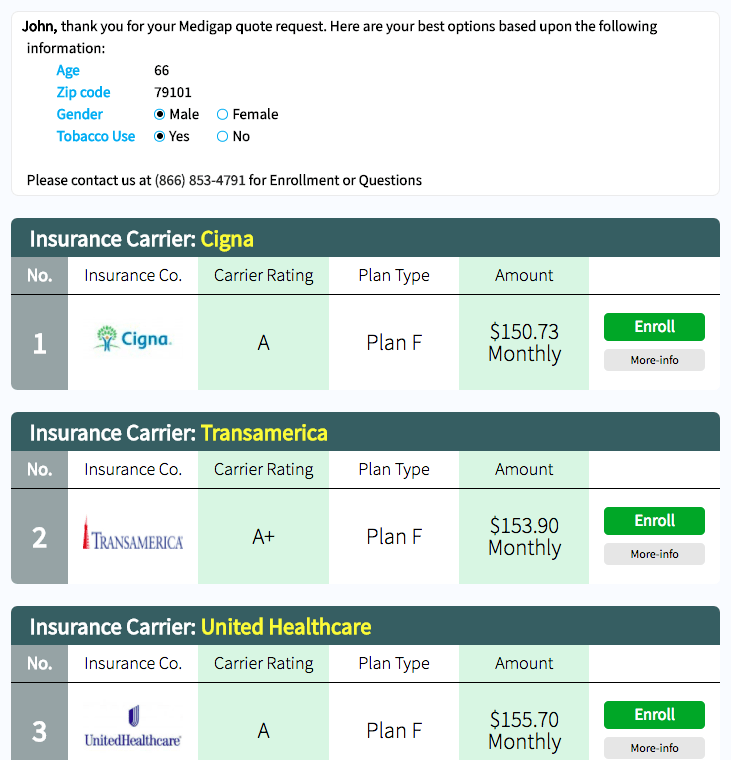
About Medigap Policies
All Medigap policies must adhere to federal and state laws designed to protect you. Each Medigap policy must be clearly identifiable as “Medicare Supplement Insurance.” In most states, insurance companies are only allowed to sell “standardized” policies that are identified by letters.
All Medigap policies offer the same basic benefits. Certain policies will offer additional benefits. This allows for individuals to choose which the policy that best suits their personal needs. Medigap policies in Wisconsin, Massachusetts and Minnesota use alternate standardization methods.
Insurance companies decide the Medigap policies they desire to sell. However, state laws may affect the policies they are able to offer.
These rules apply to insurance carriers that sell Medigap policies:
- It is not necessary to offer every Medigap plan
- If an insurance company offers any Medigap policy then they must offer Medigap Plan A
- The insurance carrier must also offer either Plan C or Plan F
The Medigap policies will only cover coinsurance once the deductible has been met. The exception to this would be if the Medigap policy specifically includes deductible coverage.